Now, a 'safe' immunotherapy offers hope for cancer patients with HIV
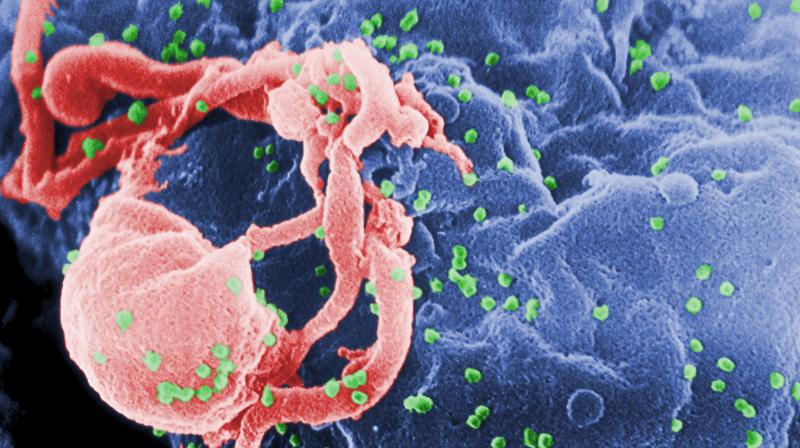
Washington DC: A new category of immunotherapies, called checkpoint inhibitors, appears safe to use in patients with both advanced malignancies and HIV, according to a recent study.
Principal Investigator Thomas Uldrick of the HIV & AIDS Malignancy Branch at the National Cancer Institute, will present late breaking results from the first 17 patients on a phase I study of pembrolizumab in patients with HIV and advanced cancers at the Society for Immunotherapy of Cancer's annual meeting in National Harbor, Maryland.
"During the development of these drugs, people with HIV were routinely excluded from studies due to concerns that they would not tolerate these medications or perhaps not benefit from them because of their underlying HIV and associated immune dysfunction," Uldrick said. "The most important first step was to show that this class of drug would be safe in cancer patients with HIV."
Study participants, who were on standard antiretroviral therapy to control their HIV infections and had various cancers that had failed to respond to standard therapies, received pembrolizumab (Keytruda), known since 2015 as "the Jimmy Carter drug" after it swiftly beat back melanoma that had spread to the former president's brain and liver.
"These drugs are the backbone of cancer immunotherapy at present and have been shown to be effective in subsets of virtually every different kind of cancer," said senior author Martin "Mac" Cheever. "For patients with HIV who are using effective antiretroviral therapy and have cancers for which these drugs are approved, there's no reason not to consider these drugs as standard therapy."
From the earliest days of the AIDS pandemic, Kaposi sarcoma -- a rarely seen cancer until then -- was one of a trio of cancers known as AIDS-defining malignancies. It, non-Hodgkin lymphoma and, in women, cervical cancer, often signaled that a person's HIV infection had progressed to full-blown AIDS. People did not die of AIDS, per se. They died of one of these cancers or of infections like pneumocystis pneumonia and toxoplasmosis that took advantage of a weakened immune system.
The ongoing study will enroll up to 36 patients, and there are plans to include more patients with Kaposi sarcoma, a cancer for which checkpoint inhibitors have not been studied. It is one of the leading causes of cancer deaths in sub-Saharan Africa -- where HIV rates are high -- and new treatments are sorely needed.
Also to be presented Friday is the death of one patient later in the study who had Kaposi sarcoma. The death is still being evaluated but was likely due to dissemination of KSHV. Uldrick and Cheever said review of the case suggests the patient had a history of symptomatic KSHV viremia, and the study has been changed to exclude such patients in the future and provide specific guidelines for management should new symptomatic KSHV viremia be observed.
Six other study participants with Kaposi sarcoma or primary effusion lymphoma have been treated on this study. None has experienced similar problems, and some have benefitted from therapy, Uldrick said.
"We do not believe that this takes away from the safety message in patients with HIV and other, better studied cancers," Uldrick said. "However, more experience is clearly needed in treating KSHV-associated diseases with checkpoint inhibitors."

