Government Draft Bill riddled with drawbacks
Where a patient is suffering from terminal illness, there is the aspect of End Of Life Care which the Bill has not considered.
The Government of India has solicited public opinion and comments for the formulation of a law on “passive euthanasia”. Along with the Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill, the ministry of health and family welfare (MoHFW) also uploaded an explanatory note along with a brief on euthanasia on its website.
In the Aruna Shanbaug case, the Supreme Court held that passive euthanasia, which involves withdrawal of life-saving measures, is permissible even without any supporting legislation, provided certain conditions are met and safeguards observed.
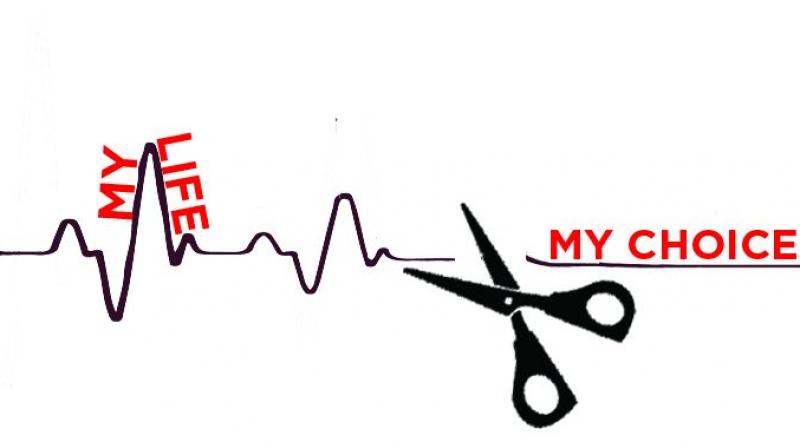
In the case of Gian Kaur vs State of Punjab, the SC held that every person has a right to die with dignity and the same is enshrined under Article 21 of the Constitution of India. Despite this recognition, the Bill introduced by the MoHFW falls short of providing the right to a dignified death.
The focus of the Bill is on passive euthanasia. Where a patient is suffering from an incurable and irreversible terminal illness, there is a much larger aspect of End Of Life Care, which the Bill has not considered. Among the many major drawbacks of the Bill are the inadequate definitions of “advance medical directives” and “medical power of attorney”. A living will or advance medical directive or medical power of attorney represents the patient’s wishes in case he or she becomes incapacitated due to a terminal illness or otherwise. The Bill has invalidated both. Withdrawal/withholding decisions are based on respect to the individual choice of treatment made by patients towards End Of Life Care. It’s time, we as a society recognise the concept of living wills, medical power of attorney(s) and advance medical directives whereby a person can draw up such a document while he is physically fit and of sound mind.
Secondly, Section 3 of the Bill provides for refusal of medical treatment by a competent patient (including a minor aged above 16) and its binding nature on the medical practitioners. No reason has been provided for this. The benefit of this section should be available to patients of all ages.
According to Section 3(3) of the Bill, before giving effect to the decision of a competent patient, the medical practitioner shall not give effect to such a decision for a period of three days following the intimation given to the patient’s relatives. From a medical perspective, there is a belief that there is no reason why there should be a delay of three days in implementing the wishes of a competent patient.
Also, Section 5 provides for the medical practitioner to maintain records and inform the patient’s parents. This provision is in conflict with Sections 3 and 8. This provision states about the request or decision, if any, communicated by the “patient and his opinion”. This means that any patient (competent or incompetent) can communicate his decision to withdraw or withhold treatment and if he does, then the medical practitioner shall inform the patient (if conscious) and the spouse, parent or major son or daughter of the patient etc. If the family opinion is not necessary for an incompetent patient, why should this be important for a competent patient? What if the patient has no family or friends or is incompetent and without family?
Then, Section 6 provides for Palliative Care. This section is in conflict with Section 3, which only permits a competent patient to refuse medical treatment. How will an incompetent patient give consent to withhold or withdraw consent? This section provides that even though medical treatment has been withheld or withdrawn by the medical practitioner in accordance with the Bill, such a practitioner is not debarred from administering Palliative Care.
This section is correct in letter as well as spirit. But the earlier provisions of the Bill do not allow incompetent patients to take any decision about withholding or withdrawing treatment. The expression in this section is against ethical principles of the medical fraternity, as the treating physician is in fact obliged to offer Palliative Care and emotional support to the patient and his family.
Section 7 affords protection of competent patients from criminal action. In case the decision is taken by the patient along with his family members and consequently it is the family members who need the immunity, this is a major shortcoming.
Section 8 provides for protection of medical practitioners and others acting under their direction, in relation to competent and incompetent patients. This provision cannot apply as this is in the context of terminal illness and the right to an informed choice in the matter of medical treatment.
A provision such as Section 9 of the Bill, which provides for permission to be obtained from the High Court, should only come into play in cases of disputes. Rights of the patient remain intact even when the patient is incompetent. Shared decision-making between the physician and family should remain intact. These are complex medical decisions based on bedside understanding of the prognosis and communication between physician’s team and the patient’s kin. This cannot be duplicated in the High Court. This is impractical.
Currently, there is no law related to End Of Life Care in India. Usually, it’s the patient’s family members who end up taking critical decisions. The emphasis has always been on quantity of life over quality of life. It’s time we recognise that the patient autonomy is of paramount importance. Hence, the proposed law has to recognise this and make it the basis for the new law. After all, everyone must have the right to End Of Life Care and a dignified death, as guaranteed under our Constitution.
Die-hard Facts
Netherlands: Allows physician assisted death under strict conditions if person is suffering unbearable pain, incurable illness and has made plea in full consciousness.
United States: Doctors can administer lethal drugs to patients in five states in the country.
Germany: In 2010, Germany’s Federal Court of Justice ruled that cutting off life support for consenting, terminally-ill patients is not a crime. Passive physician assisted dying is also legal if death is inevitable.
Switzerland: Physician-assisted suicide is sanctioned as long as there is no “self-seeking” motive. It also has organisations which provide assisted dying service for a fee.
Belgium: Passed a law in 2002, which states that doctors can assist patients to end their lives if they are suffering from terminal illness, unbearable pain.
Luxembourg: Patients suffering from incurable, unbearable physical/mental pain, can end their life with the help of a doctor.
(The author is a partner at DSK Legal, Mumbai. He is a solicitor registered with Bombay Incorporated Law of Society and qualified as solicitor from Supreme Court of England & Wales. He is registered to practice with the Bar Council of Maharashtra and Goa.)

